 |
|

For Providers
|
July 2024 |
| |
NEWS & UPDATES |
|
New Coupe Health Plan: Update Your Member Records
Starting in October 2024, providers in our commercial PPO network may see members of our new Coupe Health benefit plan. You won’t collect any copay from Coupe Health plan members.
|
|
|
|
Updates made to the Provider Reference Manual
The Provider Reference Manual  from Blue Cross and Blue Shield of New Mexico has been updated, effective Aug. 3, 2024. Changes to the PRM include, but are not limited to, the following sections: from Blue Cross and Blue Shield of New Mexico has been updated, effective Aug. 3, 2024. Changes to the PRM include, but are not limited to, the following sections:
| • |
4 — Professional Provider Responsibilities |
The updated PRM is available on the Provider Reference Manual webpage. BCBSNM reminds providers to review the PRM for all changes.
|
|
 |
Reminder
|
|
|
|
 |
| |
EDUCATION & REFERENCE |
|
Cultural Awareness Webinars: No-Cost Continuing Education Credit
We offer a suite of no-cost webinars that provide cultural awareness training and continuing education credit.
|
|
|
|
Coming Soon — New Learning & Training Center in Availity® Essentials
Starting in August 2024, some of the educational resources on our Provider website are moving to a new Learning & Training Center within Availity Essentials.
|
|
|
 |
Reminder
|
|
|
|
 |
| |
NETWORK PARTICIPATION |
|
Member Rights and Responsibilities
As a participating provider, it’s important that you are aware of our members’ rights and responsibilities.
|
|
|
|
Provider Rights and Responsibilities
As a participating provider, you have certain rights and responsibilities that may affect your practice.
|
|
|
|
| |
CODING AND CLAIMS |
|
Prior Authorization Requests May Be Needed Due to Pharmacy Claims Processing Error
A system error resulted in some members, with Prime Therapeutics as their pharmacy benefit manager, receiving paid claims without following the necessary prior authorization steps. The error has been fixed. Affected members may now need prior authorization approval for continued coverage of their drug.
|
|
|
|
Clinical Payment and Coding Policy Updates
The Clinical Payment and Coding Policies on our website describe payment rules and methodologies for CPT, HCPCS and ICD-10 coding for claims submitted as covered services. This information is a resource for our payment policies. It is not intended to address all reimbursement-related issues. We regularly add and modify clinical payment and coding policy positions as part of our ongoing policy review process.
The following policies were updated:
| • |
CPCP010: Anesthesia Information — Effective 01/01/25 |
| • |
CPCP024: Evaluation and Management Coding – Professional Provider Services — Effective 09/01/24 |
|
|
|
Our Revised Clinical Payment and Coding Policy for Anesthesia Services Is Now Effective Jan. 1, 2025
What’s changing?
Now effective Jan 1, 2025, we are updating our Clinical Payment and Coding Policy, Anesthesia Information (CPCP010).
The details
Under this revised policy we will no longer offer additional reimbursement for services based on the use of physical status (P code) modifiers when appended to anesthesia services.
What do I need to do?
Review in detail the revised policy — Anesthesia Information CPCP010  . .
|
|
|
Coding Update: Reimbursement Change for Consultation Services
What’s changing?
Effective Sept. 1, 2024, we are updating our Clinical Payment and Coding Policy, Evaluation and Management Coding CPCP024.
The details
Under this revised policy we will no longer reimburse for outpatient or inpatient consultation using CPT codes 99242 - 99245 and 99252 - 99255. Consultation services should be reported with an appropriate office outpatient or inpatient evaluation and management code representing the location where the visit occurred and the level of complexity of the visit performed.
What do I need to do?
Review in detail the revised policy — Evaluation and Management Coding CPCP024  . .
|
|
|
 |
| |
CLINICAL RESOURCES |
|
Access MCG Care Guidelines Clinical Criteria via Availity
We often use select clinical criteria from MCG Care Guidelines when reviewing requests to determine medical necessity. Our clinical rationale outlined in provider correspondence and Clinical Payment and Coding Policies will guide you to the specific MCG Care Guidelines, when applicable.
|
|
|
|
Encourage Routine Vaccines and Well-Care Visits for Children and Teens
Many children and adolescents are still catching up on missed routine immunizations and well-care visits, according to the Centers for Disease Control and Prevention. The CDC recommends that doctors and health care professionals encourage families to schedule vaccines and visits for their children.
|
|
|
|
In-Home Test Kits for Colorectal Cancer Screening
We’re providing in-home test kits this summer to certain Blue Community HMOSM members who, based on our data, need a colorectal cancer screening.
|
|
|
|
Physician Performance Insights Reports Coming Soon from PEAQSM
In August, physicians eligible for our Physician Efficiency, Appropriateness, and QualitySM program can view their Physician Performance Insights in Availity Essentials. PPI reports show how physicians compare to their peers and include information on improving performance. |
|
|
|
 |
| |
BEHAVIORAL HEALTH |
|
Requests for Behavioral Health Documentation for Medicaid Members
Behavioral health providers may receive requests from BCBSNM for our Medicaid plan members’ medical records and supporting documentation. We review documentation for behavioral health services to comply with regulatory standards and gather information about our members’ care. |
|
|
|
 |
| |
PHARMACY PROGRAM |
|
2024 NM Annual NDC Drug Fee Schedule Impact and Timeline
Effective for dates of service on and after Aug. 1, 2024
We review our National Drug Code Fee Schedule on an annual basis. Reimbursement rates for some medications may change because of this review. Effective Aug. 1, 2024, NDC rate changes will go into effect at BCBSNM.
To evaluate the changes in your reimbursement that may result from the updated NDC Fee Schedule, you may receive an interactive copy of the Schedule by submitting a Fee Schedule Request Form  found on bcbsnm.com/provider on or after Aug. 1, 2024. The Schedule is confidential and proprietary information and must be maintained as such per your Agreement. found on bcbsnm.com/provider on or after Aug. 1, 2024. The Schedule is confidential and proprietary information and must be maintained as such per your Agreement.
BCBSNM values your participation in our programs and welcomes your input. If you have any questions or concerns, please contact your Network Services Provider Representative  . .
|
|
|
GLP-1 New to Therapy Optional Benefit Program Available for Select Commercial Members
As of April 1, 2024, there is a new optional pharmacy benefit program available for some employer groups with Prime Therapeutics called GLP-1 New to Therapy. This new program aims to reduce the drug waste and cost of care associated with beginning GLP-1 drug therapy.
|
|
|
|
 |
| |
BLUE CROSS MEDICARE ADVANTAGESM |
|
Notify Us If You Opt Out of Medicare
As a reminder, providers with the Blue Cross Medicare Advantage plan who choose to opt out of Medicare should immediately notify their network representative with BCBSNM. In compliance with Centers for Medicare & Medicaid Services policy, we are required to terminate providers from our Medicare Advantage networks if they’ve opted out of Medicare.
|
|
|
|
 |
| |
TURQUOISE CARE |
|
New Mexico Medicaid Extends Support to Members Affected by Ruidoso Evacuations
The New Mexico Human Services Department and Medicaid Managed Care Organizations are here to assist members impacted by the Salt Fire and South Fork Fire.
|
|
|
|
New Mexico Medicaid Shares Update on Provider Rates
The New Mexico Human Services Department has provided details on the state’s current provider rates.
|
|
|
|
Resources for Providers Needing Language Assistance for Members
Providers with BCBSNM for Medicaid managed care must provide an interpreter when a Medicaid member to whom they are furnishing covered services needs language assistance. Providers who want support from BCBSNM in arranging these services can visit the language assistance page on bcbsnm.com that is linked in the top right corner of every page or call 1-855-710-6984.
Please refer to the Medicaid Provider Reference Manual for additional information or contact your Provider Representative using the Network Contact List  . .
|
|
|
Keep Your Enrollment Status with New Mexico Medicaid Updated
Medicaid providers should ensure their Enrollment Status with New Mexico Medicaid is up to date. Failure to comply with these requirements may result in termination from the New Mexico Medicaid program and denial of claims.
|
|
|
|
Billing Tips for Midwife Providers
We have tips for billing midwifery services furnished to Medicaid members in licensed birth centers and as home births.
|
|
|
|
Prenatal and Postpartum Care Coordination Changes for Medicaid Members
As part of Turquoise Care, community-based organizations and maternity providers began managing prenatal and postpartum care coordination for our Medicaid members as of July 1, 2024.
|
|
|
|
 |
| |
BCBSNM IN THE COMMUNITY |
|
BCBSNM, Eastern New Mexico University and National Fitness Campaign Prioritize Health and Wellness for the ENMU Community
BCBSNM and the National Fitness Campaign have partnered with Eastern New Mexico University to bring an outdoor Fitness Court® and digital wellness program to their campus. |
|
|
|
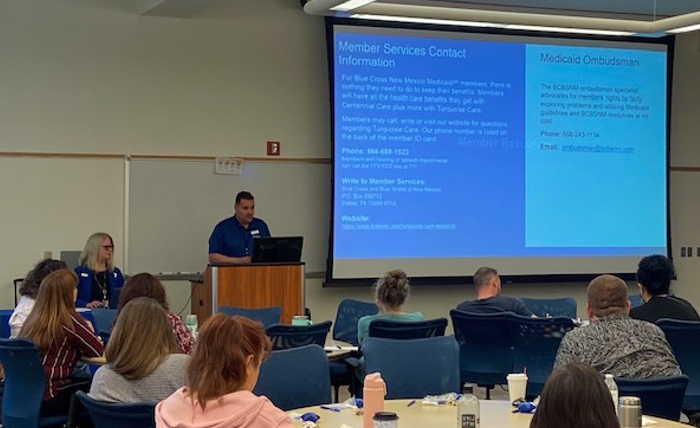
Provider Engagement at BCBSNM
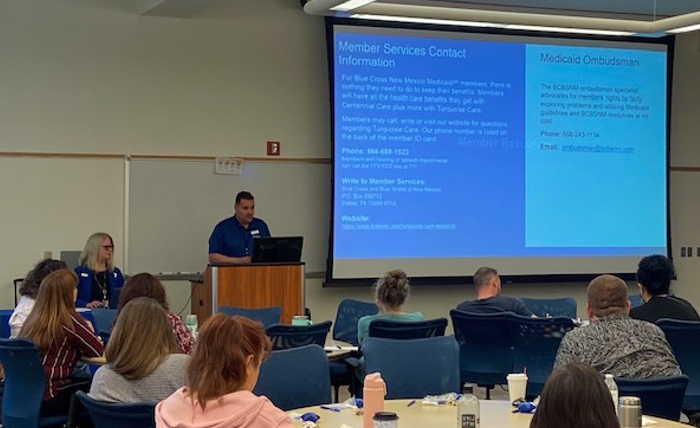
New Mexico Medicaid Providers attended a Turquoise Care training hosted by the Provider Network team on May 21. The Provider Network team hosted trainings in May and June throughout the state. |
|
|
 |
 |
Not Yet Contracted?
Providers who are participating in commercial products of BCBSNM are not automatically participating providers in Turquoise Care. If you are interested in becoming a provider of Turquoise Care, please call 505‑837‑8800 or 800‑567‑8540.
|
|
 |
 |
Reminder: Update your Enrollment Information
Due to Turquoise Care requirements, all enrollment information (changes to demographics, licensure or certification, provider status, etc.) must be updated on the NM Medicaid Provider Web Portal  . .
Visit our Website
It’s important for you to stay informed about news that could affect your practice. BCBSNM offers many ways to stay informed via our website, bcbsnm.com/provider, and our provider newsletter, Blue Review. Signing up is easy.
|
|
 |
 |
Medical Policy Updates
Approved new or revised medical policies and their effective dates are usually posted on our website the 1st and 15th of each month. These policies may impact your reimbursement and your patients’ benefits. These policies  are located under the Standards & Requirements tab at bcbsnm.com/provider. are located under the Standards & Requirements tab at bcbsnm.com/provider.
Clinical Payment and Coding Policies
BCBSNM has adopted additional clinical payment and coding policies. These policies are based on criteria developed by specialized professional societies, national guidelines (e.g. Milliman Care Guidelines and the CMS Provider Reimbursement Manual and are not intended to provide billing or coding advice but to serve as a reference for facilities and providers. These policies are located under the Standards & Requirements tab at bcbsnm.com/provider.
Claims Inquiries
Our Provider Service Unit handles all provider inquiries about claims status, eligibility, benefits and claims processing for members of BCBSNM. To contact the PSU for BlueCard® within BCBSNM, call 800‑222‑7992. For out‑of‑area claims inquiries, call 888‑349‑3706.
Network Services Contacts and Related Service Areas
|
|
 |
 |
Verify Your Directory Details & Look for Reminders
Your directory information must be verified every 90 days under a new federal law. It’s easy and quick to get it done for all health plans in Availity®  , or if you prefer, you can use our Demographic Change Form. If we haven’t received your verification, look for emails and postcards from us with the checkmark symbol , or if you prefer, you can use our Demographic Change Form. If we haven’t received your verification, look for emails and postcards from us with the checkmark symbol  . They’re a friendly reminder that it’s time to verify or update. . They’re a friendly reminder that it’s time to verify or update.
Member Rights and Responsibilities
Policies at BCBSNM help address the issues of members participating in decision making regarding their treatment; confidentiality of information; treatment of members with dignity, courtesy and a respect for privacy; and members’ responsibilities in the practitioner‑patient relationship and the health care delivery process.
|
|
 |
|
|
|
 File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com  . .
 By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy. By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.
Availity is a trademark of Availity, L.L.C., a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSNM.
|
Blue Cross and Blue Shield of New Mexico, a Division of Health Care Service Corporation,
a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association
|
5701 Balloon Fiesta Pkwy NE, Albuquerque, NM 87113
© Copyright 2024 Health Care Service Corporation. All Rights Reserved.
Legal and Privacy | Unsubscribe
view in Web Browser
|
|
|













![]() File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com
File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com ![]() .
.![]() By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.
By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.