 |
|

For Providers
|
December 2023 |
| |
NEWS & UPDATES |
|
COVID-19 Information for Providers
Please check the following Blue Cross and Blue Shield of New Mexico resources frequently for updates to important information related to COVID-19.
|
|
|
Updates made to the Provider Reference Manual
The BCBSNM Provider Reference Manual  has been updated as part of an annual review, effective Jan. 1, 2024. Changes to the PRM include, but are not limited to, the following sections: has been updated as part of an annual review, effective Jan. 1, 2024. Changes to the PRM include, but are not limited to, the following sections:
| • |
1 — Contact Information |
| • |
2 — Introduction |
| • |
3 — Network Services |
| • |
4 — Professional Provider Responsibilities |
| • |
6 — Facility and Ancillary Providers |
| • |
7 — Member Information |
| • |
8 — Claims |
| • |
9 — Electronic Commerce Tools |
| • |
10 — Prior Authorization and Recommended Clinical Review |
| • |
11 — Utilization, Case, Population Health, And Condition & Lifestyle Management |
| • |
12 — Behavioral Health Services |
| • |
14 — Pharmacy Services |
| • |
15 — Provider Service Inquiry and Grievance Process |
| • |
16 — Credentialing |
| • |
17 — Quality Improvement |
The updated PRM is available on the Provider Reference Manual webpage. BCBSNM reminds providers to review the PRM for all changes.
|
|
|
|
| |
 |
Reminder
|
|
 |
| |
EDUCATION & REFERENCE |
|
Chronic Kidney Disease Management Strategies for Primary Care Providers
BCBSNM invites primary care providers to an online learning series on chronic kidney disease management strategies. The courses offer continuing medical education credit at no cost to you. |
|
|
|
 |
|
|
| |
 |
Reminder
|
|
 |
| |
CODING AND CLAIMS |
|
Reimbursement Rate Update for Some Commercial ABA Codes
Effective Jan. 1, 2024, Blue Cross and Blue Shield of New Mexico will update the reimbursement rates for the ABA codes 0362T and 0373T.
The fee schedule will reflect the update for this code. This update applies to the following networks:
| • |
Federal Employee Program® (FEP®) |
| • |
Participating (PAR) |
| • |
Point of Service (POS) |
| • |
Preferred Provider Option (PPO) |
| • |
Health Maintenance Organization (HMO) |
| • |
Exclusive Provider Network (EPN) |
You may request an interactive copy of the fee schedule by following the steps on our Reimbursement Calculations page. Please contact your BCBSNM Provider Network Representative  if you have any questions. if you have any questions.
|
|
|
New Email Address for Electronic Commerce Services
The email address for BCBSNM Electronic Commerce Services has recently been updated to ecommerceservicesNM@bcbsnm.com.
Electronic Commerce Services is here to you assist with the following:
| • |
Electronic Remittance Advice (835 ERA) and Electronic Funds Transfer (835 EFT) Enrollment questions or issues |
| • |
Missing or out of balance 835 ERA transactions |
| • |
837 Electronic claims rejections without a claim number assigned |
| • |
Electronic Data Interchange Clearinghouse |
Please update your records with the new email address. For your convenience, inquiries sent to the previous Electronic Commerce Services email address will be forwarded to the new email address during this transition. Additionally, we are in the process of updating our provider website, forms, and provider manual with the new email address.
Not enrolled for 835 ERA and/or 835 EFT? Complete the online guided registration process via Availity® Essentials. For more information, refer to the instructional EFT and ERA Enrollment User Guide  on our provider website. on our provider website.
|
|
|
See Updates to Claim Editing Changes for Emergency Department Services
BCBSNM will enhance our claims editing and review process with Cotiviti for emergency department evaluation and management services for our commercial members. These editing enhancements for facility and professional claims will help ensure accurate billing and proper reimbursement.
|
|
|
|
 |
| |
CLINICAL RESOURCES |
|
Encourage Annual Eye Exams for Members with Diabetes
People with diabetes are at a higher risk of vision loss and eye diseases. Early diagnosis and proper treatment can greatly lower the chance of blindness from diabetic retinopathy. You may play an important role in supporting our members with diabetes by encouraging an annual retinal or dilated eye exam by an eye care specialist.
|
|
|
|
Clinical Payment and Coding Policy Updates
The Clinical Payment and Coding Policies on our website describe payment rules and methodologies for CPT, HCPCS and ICD-10 coding for claims submitted as covered services. This information is a resource for our payment policies. It is not intended to address all reimbursement-related issues. We regularly add and modify clinical payment and coding policy positions as part of our ongoing policy review process.
The following policies were updated:
| • |
CPCP005: Home Health Care/Private Duty Nursing Policy — Effective 11/3/23 |
| • |
CPCP006: Preventive Services Policy — Effective 11/1/23 |
| • |
CPCP008: Psychological and Neuropsychological Testing — 11/16/23 |
| • |
CPCP018: Outpatient Facility and Hospital Claims: Revenue Codes Requiring Supporting CPT, HCPCS and/or NDC Codes — 11/3/23 |
| • |
CPCP019: Home Infusion — 11/3/23 |
| • |
CPCP023: Modifier Reference Policy — 11/3/23 |
| • |
CPCP029: Medical Record Documentation — 11/3/23 |
| • |
CPCP036: Medical Record Documentation — 11/3/23 |
|
|
|
 |
| |
BEHAVIORAL HEATLH |
|
Training Resources for Behavioral Health Care
More than 120 million Americans live in areas experiencing a shortage in behavioral health care providers. Even when providers are available, patients often rely on primary care physicians for behavioral health care. BCBSNM has compiled resources that providers across disciplines may find helpful to support patients presenting with behavioral health concerns.
|
|
|
|
 |
| |
PHARMACY PROGRAM |
|
Pharmacy Program Quarterly Update Changes Effective Jan. 1, 2024 — Part 1
Based on the availability of new prescription medications and Prime’s National Pharmacy and Therapeutics Committee’s review of changes in the pharmaceuticals market, some additions or drugs moving to a lower out-of-pocket payment level, revisions (drugs still covered but moved to a higher out-of-pocket payment level) and/or exclusions (drugs no longer covered) were made to the Blue Cross and Blue Shield of New Mexico drug lists. Your patient(s) may ask you about therapeutic or lower cost alternatives if their medication is affected by one of these changes.
View the Pharmacy Program Updates effective as of Jan. 1, 2024. 
|
|
|
 |
| |
BLUE CROSS MEDICARE ADVANTAGESM (MEDICARE) |
|
Updates Made to the Blue Cross Medicare Advantage Provider Reference Manual
The Blue Cross Medicare Advantage Provider Reference Manual  has been updated as part of an annual review, effective Jan. 1, 2024. Changes to the PRM include, but are not limited to, the following sections: has been updated as part of an annual review, effective Jan. 1, 2024. Changes to the PRM include, but are not limited to, the following sections:
| • |
1 — Introduction |
| • |
4 — Benefits and Member Rights |
| • |
5 — Selection and Retention of Providers |
| • |
6 — Performance and Compliance Standards |
| • |
7 — Utilization Management |
| • |
8 — Case Management |
The updated PRM is available on the Provider Reference Manual webpage. BCBSNM reminds providers to review the PRM for all changes.
|
|
|
Medical Records Reminder for Out-of-Area Medicare Advantage Members
If we need medical records for Blue Cross Group Medicare Advantage (PPO)SM members, you will receive requests from BCBSNM or our vendor, Change Healthcare, as part of the Blue Cross and Blue Shield National Coordination of Care program. In addition, you may receive requests from EXL Health for select inpatient, diagnosis-related group claims for any out-of-area Blue Cross Medicare Advantage members.
Please respond promptly to our requests so that we may in turn provide timely service to those Medicare Advantage members.
|
|
|
Blue Cross Medicare Advantage Dual Care PlusSM 2022 Program Summary
The Blue Cross Medicare Advantage Dual Care Plus program started Jan. 1, 2020. The Special Needs Plan continued in its form for a three-year period. The program serves older adults and people with disabilities. |
|
|
|
Blue Cross Medicare Advantage Dual Care Plus Preferred 2022 Program Summary
The Blue Cross Medicare Advantage Dual Care Plus Preferred program started Jan. 1, 2022. The Special Needs Plan will continue in its current form for three years. The program serves older adults and people with disabilities. |
|
|
|
 |
| |
BLUE CROSS COMMUNITY CENTENNIALSM (MEDICAID) |
|
Rate Increase for After Hours/Weekend Well Child Visits
Effective Nov. 15, 2023, BCBSNM is offering contracted providers a new revenue opportunity for Blue Cross Community Centennial members. Providers that are willing to expand their hours to accommodate help improve access to well child visits on weekends or after hours.
|
|
|
|
Updates Made to the Blue Cross Community Centennial Provider Reference Manual
The Blue Cross Community Centennial Provider Reference Manual has been updated as part of an annual review, effective Jan. 1, 2024. Changes to the PRM include, but are not limited to, the following sections:
| • |
Program Overview |
| • |
Claims |
| • |
Health Care Management |
| • |
Provider Performance Standards and Compliance Obligations |
| • |
Selection and Retention of Participating Providers |
| • |
Pharmacy Services |
| • |
Glossary of Terms |
| • |
Contact List |
The updated PRM is available on the Provider Reference Manual webpage. BCBSNM reminds providers to review the PRM for all changes.
|
|
 |
Reminder
|
|
|
|
 |
| |
BCBSNM IN THE COMMUNITY |
|
BCBSNM Will Open a Blue Door Neighborhood Center in the South Valley
BCBSNM is proud to announce that we will be opening a Blue Door Neighborhood CenterSM in Albuquerque’s South Valley. The Center will offer members and the community access to in-person resources to improve their health and wellness at no cost.
|
|
|
|
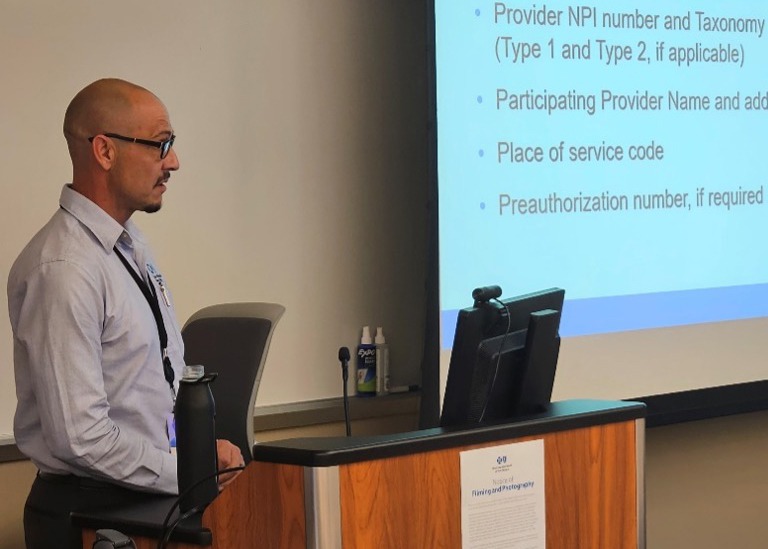
BCBSNM Provider Engagement
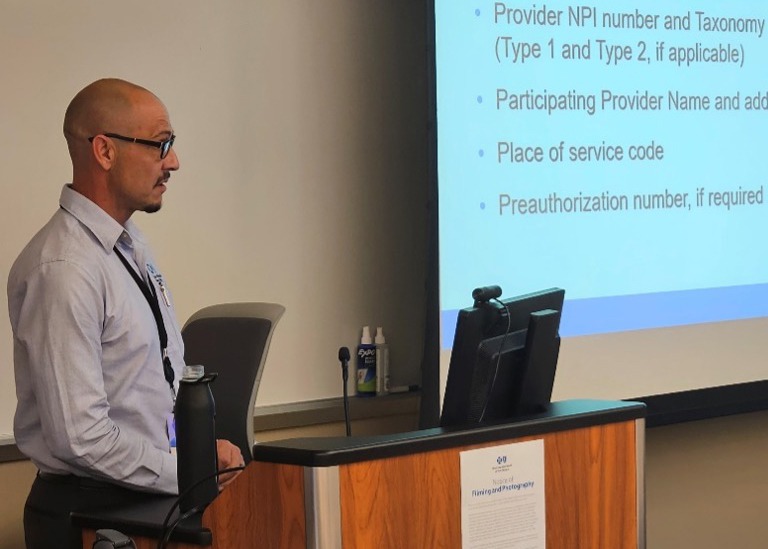
Peter Crespin, BCBSNM Provider Relations Representative, presents at BCBSNM’s annual Medicaid provider training held in Albuquerque on Oct. 25. |
|
|
 |
 |
Not Yet Contracted?
Providers who are participating in commercial BCBSNM products are not automatically participating providers in Blue Cross Community Centennial. If you are interested in becoming a Blue Cross Community Centennial provider, please call 505‑837‑8800 or 800‑567‑8540.
|
|
 |
 |
Reminder: Update your Enrollment Information
Due to Centennial Care requirements, all enrollment information (changes to demographics, licensure or certification, provider status, etc.) must be updated on the NM Medicaid Provider Web Portal  . .
BCBSNM Website
It’s important for you to stay informed about news that could affect your practice. BCBSNM offers many ways to stay informed via our website, bcbsnm.com/provider, and our provider newsletter, Blue Review. Signing up is easy.
|
|
 |
 |
Medical Policy Updates
Approved new or revised medical policies and their effective dates are usually posted on our website the 1st and 15th of each month. These policies may impact your reimbursement and your patients’ benefits. These policies  are located under the Standards & Requirements tab at bcbsnm.com/provider. are located under the Standards & Requirements tab at bcbsnm.com/provider.
Clinical Payment and Coding Policies
BCBSNM has adopted additional clinical payment and coding policies. These policies are based on criteria developed by specialized professional societies, national guidelines (e.g. Milliman Care Guidelines and the CMS Provider Reimbursement Manual and are not intended to provide billing or coding advice but to serve as a reference for facilities and providers. These policies are located under the Standards & Requirements tab at bcbsnm.com/provider.
Claims Inquiries
Our Provider Service Unit handles all provider inquiries about claims status, eligibility, benefits and claims processing for BCBSNM members. For the BCBSNM BlueCard® PSU, call 800‑222‑7992. For out‑of‑area claims inquiries, call 888‑349‑3706.
Network Services Contacts and Related Service Areas
|
|
 |
 |
Verify Your Directory Details & Look for Reminders
Your directory information must be verified every 90 days under a new federal law. It’s easy and quick to get it done for all health plans in Availity®  , or if you prefer, you can use our Demographic Change Form. If we haven’t received your verification, look for emails and postcards from us with the checkmark symbol , or if you prefer, you can use our Demographic Change Form. If we haven’t received your verification, look for emails and postcards from us with the checkmark symbol  . They’re a friendly reminder that it’s time to verify or update. . They’re a friendly reminder that it’s time to verify or update.
Member Rights and Responsibilities
BCBSNM policies help address the issues of members participating in decision making regarding their treatment; confidentiality of information; treatment of members with dignity, courtesy and a respect for privacy; and members’ responsibilities in the practitioner‑patient relationship and the health care delivery process.
|
|
 |
|
|
|
 File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com  . .
 By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy. By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.
Availity is a trademark of Availity, L.L.C., a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSNM.
|
Blue Cross and Blue Shield of New Mexico, a Division of Health Care Service Corporation,
a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association
|
5701 Balloon Fiesta Pkwy NE, Albuquerque, NM 87113
© Copyright 2023 Health Care Service Corporation. All Rights Reserved.
Legal and Privacy | Unsubscribe
view in Web Browser
|
|
|














![]() File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com
File is in portable document format (PDF). To view this file, you may need to install a PDF reader program. Most PDF readers are a free download. One option is Adobe® Reader® which has a built-in screen reader. You can download other tools and learn more about accessibility at adobe.com ![]() .
.![]() By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.
By clicking this link, you will go to a website/app (“site”). The site may be offered by a vendor or an independent third party. The site may also contain non-Medicare related information. Some sites may require you to agree to their terms of use and privacy policy.